Diagnosis of disseminated Tuberculosis in bone marrow aspirates
Dr. Alexander von Paleske 16th September 2011
Mpilo-Hospital
Teaching Hospital of the University of Zimbabwe
Department of Haematology
Bulawayo/Zimbabwe
Africa
Introduction
Disseminated /miliary TB is a lifethreatening form of Tuberculosis, not rarely see in HIV-AIDS patients with a CD4 count below 200/ul.
The diagnosis is often made on clinical grounds. Chest X-rays may show involvement of the lungs, however a final diagnosis is often difficult.
Disseminated / miliary TB can involve the bone marrow. A few studies albeit with small numbers have shown, that bone marrow aspirates may thus play a useful role in the diagnosis.
3% of all Tuberculosis cases worldwide are meanwhile multidrug resistant (MDR-TB). In certain affected areas the incidence is much higher. The extensive drug resistant TB (XDR-TB) is on the rise as well.
Thus the diagnosis of MDR-and XDR-TB becomes extremely important.
In disseminated / miliary TB it is difficult to obtain a specimen for culture, as the sputum results are often negative, and invasive procedures like lung- or liver aspirates carry a considerable risk for the patient.
The bone marrow aspirate, however carries a comparatively low risk.
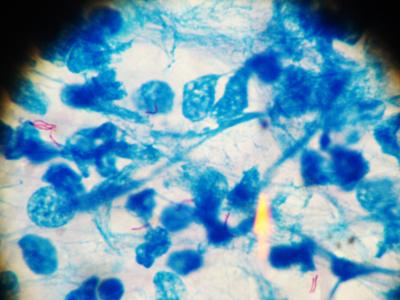
Disseminated TB - Bone marrow aspirate, Presence of AAFB's (red)
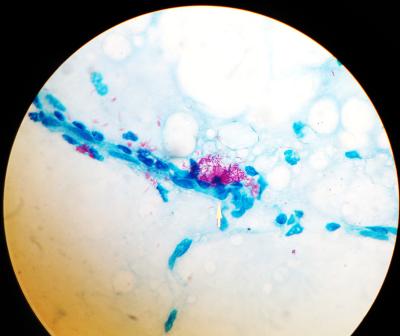
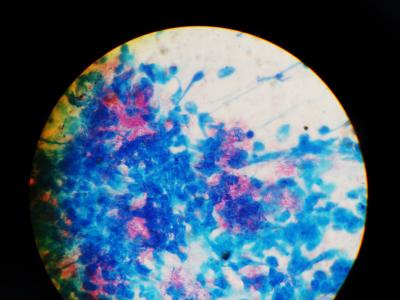
Severe disseminated TB - Two Bone marrow aspirates, plentiful AAFB's. Photos: Dr. v. Paleske
In a small pilot study (not published) in 1997 we investigated the incidence of TB-culture-positive bone marrow aspirates obtained from 30 unselected patients. One specimen was positive for m. tuberculosis.
In view of increasing numbers of MDR-TB and XDR-TB, we decided to investigate
- Whether the incidence of TB in bone marrow aspirate cultures has significantly increased and thus becomes a useful tool in the diagnosis of disseminated TB
- How frequently can Alcohol and Acid Fast Bacilli (AAFBs) be detected in bone marrow specimens and thus enabling a rapid diagnosis
- Whether or not bone marrow aspirates can be collected in simple EDTA-tubes and sent to a TB-laboratory for culture, thus enabling the sampling of bone marrow aspirates for culture even in provincial and district hospitals without access to culture mediums.
.
Patients and Methods
312 bone marrow aspirates from patients with the diagnosis of anaemia, severe granulocytopenia, thrombocytopenia, bicytopenia or pancytopenia, referred to Mpilo Hospital, Department of Haematology during the period from 1st May 2010 to 30th April 2011, were obtained.
- 186 adults, age 15-86 years (median 32 years)
- 126 children age 2 months – 14 years (median 5 years)
Bone marrow smears were stained in a conventional way, in addition one slide was stained with Ziehl-Neelsen for detection of AAFBs, and the bone marrow specimens, collected in an EDTA-tubes, then sent for TB-culture.
Results:
33 / 312 specimens were TB-culture positive ( 10,58%), all m. tuberculosis
- 6 / 126 in children ( 4,76 %)
- 27/186 in adults ( 14,5%)
Microscopically AAFBs positive were 4 /33 ( 12%) of the culture positive specimens
- 0 / 6 in children
- 4 / 27 ( 14,8 %) in adults
Patients, whose specimens were AAFBs microscopically positive were all at an advanced stage of HIV-disease.
Discussion
Bone marrow aspirates turn out to yield a comparatively high rate of TB-culture-positive results in a setting with a high incidence of HIV-disease.
The results in adults ( 14,5%) are much higher, than expected from a previous pilot study.
However It remains unclear, how high the detection rate in disseminated / miliary TB with bone marrow involvement truly is.
PCR - not available here - has shown to increase the yield compared to culture.
The now recommended Xpert MTB/ RIF-test may be quite useful for rapid detection of TB in bone marrow aspirates.
However,it cannot replace the need for TB culture to detect MDR- and XDR-TB, as it can only detect Rifampicin- resistance, which alone is not sufficient to qualify for MDR-TB.
Moreover, this test gives a false negative result, if resistance is present not aginst Rifampicin, but instead against two of the other drugs in use for first line TB-treatment (see Lancet 2011 Vol 377, 1467) .
Furthermore this test offers nothing for the detection of XDR-TB.
Not to forget the costs of that test: roughly ten times higher than the conventional tests.
Disseminated / miliary TB - or at least the uptake rate - in children is apparently much lower than in adults.
Not rarely, TB was clinically not suspected in patients, whose bone marrow aspirate turned out to be culture-positive for TB.
The microscopic detection rate of AAFBs in this study is relatively low, nevertheless useful.
Conclusions
1. Disseminated / miliary TB can be detected in bone marrow aspirates.
2. In a setting with a high incidence for HIV-disease, all bone marrow aspirates should be routinely examined for AAFB’s, and also sent for TB- culture.
3. If a culture medium is not at hand, the specimen may be sent to a TB-Laboratory in an EDTA-tube.
4. In cases of suspected disseminated / miliary TB, a bone marrow aspirate should be performed, if possible.
 Diagnosis of disseminated Tuberculosis in bone marrow aspirates - Results of a second study
Diagnosis of disseminated Tuberculosis in bone marrow aspirates - Results of a second study
 Lymph node aspirates in Tuberculosis-Diagnosis: New challenges, new solutions – a study of 156 patients
Lymph node aspirates in Tuberculosis-Diagnosis: New challenges, new solutions – a study of 156 patients
 Lymph node aspirates in Tuberculosis-Diagnosis - A third study of 549 patients
Lymph node aspirates in Tuberculosis-Diagnosis - A third study of 549 patients
References
Görgün Akpek, Shing M. Lee, David R. Gagnon, Timothy P. Cooley, and Daniel G. Wright
Bone Marrow Aspiration, Biopsy, and Culture in the
Evaluation of HIV-Infected Patients for Invasive
Mycobacteria and Histoplasma Infections -
American Journal of Hematology 67:100–106 (2001)
Lombard EH, Victor T, Jordaan A, van Helden PD.
The detection of Mycobacterium tuberculosis in bone marrow aspirate using the polymerase chain reaction. Tuber Lung Dis. 1994 Feb;75(1):65-9.
K. Ritis, S. Giaglis, S. Rafail, E. Alepopoulou, V. Tsironidou, D. Tzoanopoulos, M. Speletas,S. Ktenidou-Kartali, P. Sideras, G. Kartalis -
Diagnostic usefulness of bone marrow aspiration material
for the amplification of IS6110 insertion element in extrapulmonary
tuberculosis: comparison of two PCR techniques -
Int J Tuberc Lung Dis 9(4):455–460 (2005)
.
E-Mail: avonpaleske@yahoo.de
Mpilo-Hospital
Teaching Hospital of the University of Zimbabwe
Department of Haematology
Bulawayo/Zimbabwe
Africa
Introduction
Disseminated /miliary TB is a lifethreatening form of Tuberculosis, not rarely see in HIV-AIDS patients with a CD4 count below 200/ul.
The diagnosis is often made on clinical grounds. Chest X-rays may show involvement of the lungs, however a final diagnosis is often difficult.
Disseminated / miliary TB can involve the bone marrow. A few studies albeit with small numbers have shown, that bone marrow aspirates may thus play a useful role in the diagnosis.
3% of all Tuberculosis cases worldwide are meanwhile multidrug resistant (MDR-TB). In certain affected areas the incidence is much higher. The extensive drug resistant TB (XDR-TB) is on the rise as well.
Thus the diagnosis of MDR-and XDR-TB becomes extremely important.
In disseminated / miliary TB it is difficult to obtain a specimen for culture, as the sputum results are often negative, and invasive procedures like lung- or liver aspirates carry a considerable risk for the patient.
The bone marrow aspirate, however carries a comparatively low risk.
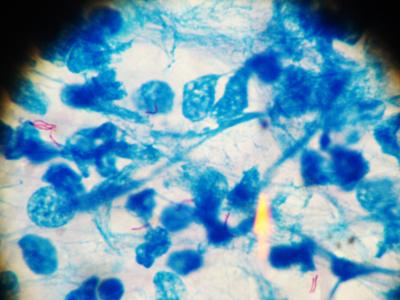
Disseminated TB - Bone marrow aspirate, Presence of AAFB's (red)
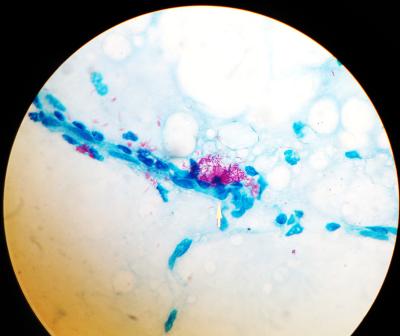
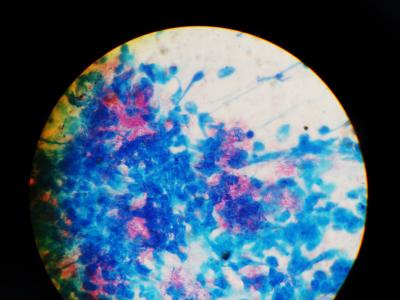
Severe disseminated TB - Two Bone marrow aspirates, plentiful AAFB's. Photos: Dr. v. Paleske
In a small pilot study (not published) in 1997 we investigated the incidence of TB-culture-positive bone marrow aspirates obtained from 30 unselected patients. One specimen was positive for m. tuberculosis.
In view of increasing numbers of MDR-TB and XDR-TB, we decided to investigate
- Whether the incidence of TB in bone marrow aspirate cultures has significantly increased and thus becomes a useful tool in the diagnosis of disseminated TB
- How frequently can Alcohol and Acid Fast Bacilli (AAFBs) be detected in bone marrow specimens and thus enabling a rapid diagnosis
- Whether or not bone marrow aspirates can be collected in simple EDTA-tubes and sent to a TB-laboratory for culture, thus enabling the sampling of bone marrow aspirates for culture even in provincial and district hospitals without access to culture mediums.
.
Patients and Methods
312 bone marrow aspirates from patients with the diagnosis of anaemia, severe granulocytopenia, thrombocytopenia, bicytopenia or pancytopenia, referred to Mpilo Hospital, Department of Haematology during the period from 1st May 2010 to 30th April 2011, were obtained.
- 186 adults, age 15-86 years (median 32 years)
- 126 children age 2 months – 14 years (median 5 years)
Bone marrow smears were stained in a conventional way, in addition one slide was stained with Ziehl-Neelsen for detection of AAFBs, and the bone marrow specimens, collected in an EDTA-tubes, then sent for TB-culture.
Results:
33 / 312 specimens were TB-culture positive ( 10,58%), all m. tuberculosis
- 6 / 126 in children ( 4,76 %)
- 27/186 in adults ( 14,5%)
Microscopically AAFBs positive were 4 /33 ( 12%) of the culture positive specimens
- 0 / 6 in children
- 4 / 27 ( 14,8 %) in adults
Patients, whose specimens were AAFBs microscopically positive were all at an advanced stage of HIV-disease.
Discussion
Bone marrow aspirates turn out to yield a comparatively high rate of TB-culture-positive results in a setting with a high incidence of HIV-disease.
The results in adults ( 14,5%) are much higher, than expected from a previous pilot study.
However It remains unclear, how high the detection rate in disseminated / miliary TB with bone marrow involvement truly is.
PCR - not available here - has shown to increase the yield compared to culture.
The now recommended Xpert MTB/ RIF-test may be quite useful for rapid detection of TB in bone marrow aspirates.
However,it cannot replace the need for TB culture to detect MDR- and XDR-TB, as it can only detect Rifampicin- resistance, which alone is not sufficient to qualify for MDR-TB.
Moreover, this test gives a false negative result, if resistance is present not aginst Rifampicin, but instead against two of the other drugs in use for first line TB-treatment (see Lancet 2011 Vol 377, 1467) .
Furthermore this test offers nothing for the detection of XDR-TB.
Not to forget the costs of that test: roughly ten times higher than the conventional tests.
Disseminated / miliary TB - or at least the uptake rate - in children is apparently much lower than in adults.
Not rarely, TB was clinically not suspected in patients, whose bone marrow aspirate turned out to be culture-positive for TB.
The microscopic detection rate of AAFBs in this study is relatively low, nevertheless useful.
Conclusions
1. Disseminated / miliary TB can be detected in bone marrow aspirates.
2. In a setting with a high incidence for HIV-disease, all bone marrow aspirates should be routinely examined for AAFB’s, and also sent for TB- culture.
3. If a culture medium is not at hand, the specimen may be sent to a TB-Laboratory in an EDTA-tube.
4. In cases of suspected disseminated / miliary TB, a bone marrow aspirate should be performed, if possible.
References
Görgün Akpek, Shing M. Lee, David R. Gagnon, Timothy P. Cooley, and Daniel G. Wright
Bone Marrow Aspiration, Biopsy, and Culture in the
Evaluation of HIV-Infected Patients for Invasive
Mycobacteria and Histoplasma Infections -
American Journal of Hematology 67:100–106 (2001)
Lombard EH, Victor T, Jordaan A, van Helden PD.
The detection of Mycobacterium tuberculosis in bone marrow aspirate using the polymerase chain reaction. Tuber Lung Dis. 1994 Feb;75(1):65-9.
K. Ritis, S. Giaglis, S. Rafail, E. Alepopoulou, V. Tsironidou, D. Tzoanopoulos, M. Speletas,S. Ktenidou-Kartali, P. Sideras, G. Kartalis -
Diagnostic usefulness of bone marrow aspiration material
for the amplification of IS6110 insertion element in extrapulmonary
tuberculosis: comparison of two PCR techniques -
Int J Tuberc Lung Dis 9(4):455–460 (2005)
.
E-Mail: avonpaleske@yahoo.de
onlinedienst - 16. Sep, 22:51 Article 10018x read