Lymph node aspirates in Tuberculosis-Diagnosis: New challenges, new solutions – a study of 156 patients
Dr. Alexander von Paleske 30 August 2011
Mpilo-Hospital
Teaching Hospital of the University of Zimbabwe
Bulawayo/Zimbabwe
Africa
Introduction
Lymph node tuberculosis is not infrequent in Sub-Saharan Africa. Even though precise figures do not exist, the incidence can be estimated to be between 10 and 25% of all TB cases..
A few studies have been published which show the value of fine needle aspiration for the diagnosis of lymph node TB, albeit with small numbers. The results were, apart from a few exceptions based on microscopy only.
In the meantime new challenges have arisen:
1. 3% of all Tuberculosis cases worldwide are multidrug resistant (MDR-TB), in certain affected areas the percentage is, however, much higher. Thus the diagnosis for MDR-TB in lymph node TB becomes extremely important. The extensive drug resistant TB (XDR-TB) is on the rise as well..
2. The HIV epidemic has brought more challenges for the diagnosis of lymph node TB
- Many patients present with enlarged lymph nodes of which it is unclear, whether this is TB, or persistent generalized HIV-related lymph node enlargement
- Other infectious diseases like Histoplasmosis and Cryptococcal infections, or simple bacterial lymphadenitis can present with lymph node enlargement as well
- The same applies to HIV-related cancers presenting with lymph node enlargement (Kaposi-Sarcoma, high grade Non Hodgkin lymphoma, Hodgkin´s disease, Castleman's disease).
- HIV-positive patients, who are on anti-TB-treatment (ATT) for lymph node TB, and who have been started concurrently or shortly before on treatment with antiretroviral drugs, can show increasing, or at least persistent lymph node enlargement, which may be in fact not drug resistant TB, but part of an Immune-Reconstitution Syndrome (IRS) or newly developed high grade lymphoma.
- The new WHO recommendations for TB-prophylaxis in HIV-positive patients - INH for a period of at least 6 months - require the exclusion of active TB, which is clinically often not possible in view of the frequently enlarged lymph nodes in HIV-positive patients.
The gold standard for a definitive diagnosis is certainly a lymph node biopsy. However this is in most of Sub-Saharan Africa, due to lack of facilities and manpower, at present only feasible for a very small number of patients.
Lymph node aspirates on the other hand are simple to perform, the specimen obtained can easily be spread on slides and then assessed by a laboratory technologist .
However, the microscopy result is often negative for TB-bacilli (AAFBs, Alcohol and Acid fast Bacilli), especially in fairly immune-competent patients, unlike with sputum in cases of TB lung,.
Helpful in the diagnosis of lymph node TB, despite the absence of microscopically detectable TB-Bacilli, is the detection of caseous material and / or the presence of Langhans giant cells.
,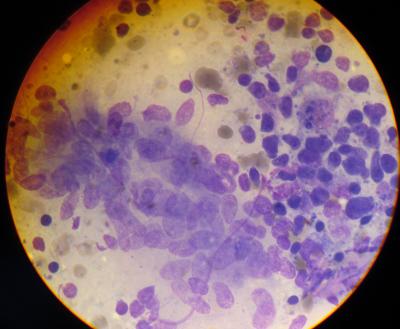
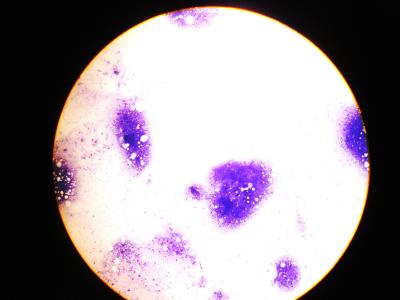
Langhans Giant cell in a lymph node aspirate - Photo: Dr. v. Paleske
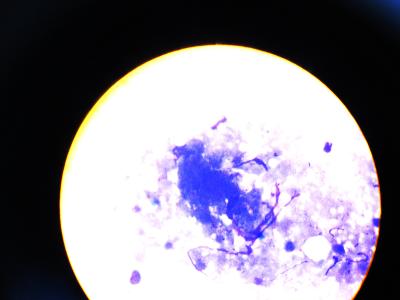
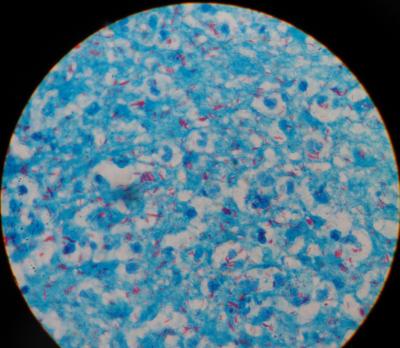
Caseous material in lymph node aspirate - Photos: Dr. v. Paleske
In our setting 25% of all lymph node aspirate specimens were falling into this category (unpublished data.). Culture of these aspirates would help further in the diagnosis of TB
In contrast: the lymph node aspirates of severely immune-compromised patients are often pus-like, packed with AAFBs and can thus fairly easily be diagnosed under the microscope.
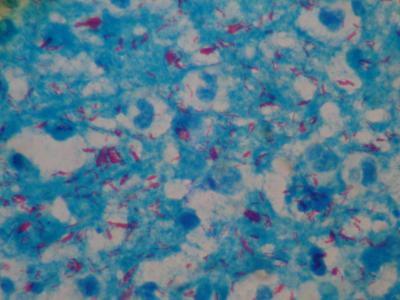
Lymph node TB, plentiful AAFBs, full blown AIDS - Photo: Dr. v. Paleske
Moreover, In view of the increasing numbers of MDR-TB and XDR-TB, culture and sensitivity testing should be done, whenever possible.
The problems: amount of specimen and mode of transport / culture medium.
For lymph node aspirates this poses a challenge, as the amount of specimen obtained with a fine needle aspirate is often little. Moreover TB-culture-medium is not available in district hospitals and clinics.
We have investigated a way to solve this problem, which allows the aspirate firstly to be spread on a slide for microscopy diagnosis and also sent off for TB culture as well.
Patients and methods
129 patients age 15 – 85 years and 27 pat. age 2 months to 14 years were referred to Mpilo-Hospital Bulawayo / Zimbabwe for fine needle aspirate of enlarged peripheral or paraarotic/parailiacal/abdominal lymph nodes during the period from 1st May 2010 to 30th April 2011.
None of the patients had a formal lymph node biopsy before.
Aspirates were performed with a 5ml or 10 ml syringe. For peripheral lymph nodes size 18 or 19 G needles were used, however for abdominal or paraaortal /parailiacal lymph node aspirates the smaller size 21 G needles.
The specimens were spread on a glass slide and a quash smear with another glass slide facilitated. This technique is better in preserving fragments and thus allows better the recognition of caseous material.
Thereafter a blood sample was taken from the patient and 1 - 1,5ml blood filled in an EDTA-Tube (Full blood count tube).
The aspirate syringe with the aspirate needle on top was flushed several times with the blood in the EDTA-tube by sucking the blood into the aspirate syringe an pressing it back into the EDTA tube, thus delivering the rest of the specimen into the EDTA-tube.
The EDTA tube was then sent to the TB-Lab for TB-culture.
May- Gruenwald Giemsa staining was being done on one glass slide, Ziehl-Neelsen for detection of AAFBs on the other.
Results
Altogether the diagnosis TB was made in 79 of the 156 specimens (50.6%)
1. Microscopically positive for TB (Langhans Giant Cells and / or caseation and / or AAFBs detected) were 62 / 79 (78,4%), of which 36 / 79 (45%) were microscopically AAFBs-positive
2. TB-Culture positive were 52/79 (65,8% of all TB diagnoses) all m. tuberculosis.
In Detail:
-- Culture positive, plus microscopically positive including AAFBs detected were 27 / 79 (34,1%)
- Culture positive plus microscopically caseation and / or Langhans giant cells but no AAFBs microscopically detected were 12 / 79 (15,1%)
- Culture positive “only” , microscopically no evidence of TB (neither AAFB's detected, nor caseation, nor Langhans giant cells were found, instead a reactive pattern) was seen in 13 / 79 specimens (16,4%)
- Culture negative but microscopically positive plus AAFBs detected were 9 /79 (11,3%)
- Culture negative, but microscopically positive however no AAFBs detected were 18 / 79 (22,7%)
Discussion
The aspirate-specimens from lymph nodes mixed with 1-1,5 ml of EDTA-Blood from the patient, had an acceptable yield.
We, however, did not separate the patients, who are on Anti TB drugs, and for how long, or not at all.
Patients, whose aspirates are microscopically AAFB´s negative, culture negative but were diagnosed on the basis of caseation, or pus, or Langhans giant cells, without the presence of Non-TB bacilli, and without a significant amount of granulocytes or macrophages, who are either for weeks on anti-TB-drugs or have recently completed their TB treatment cannot outright be regarded as therapeutic failures.
Therefore a change of treatment (switch to 2nd line TB treatment) seems not justified, rather a “wait and see policy” should be pursued with a second aspirate in due course.
.
Those however, whose aspirates are microscopically AAFBs positive, not on ATT and culture negative are definitely culture falsely negative and need treatment. A repeat aspirate solely for culture may be appropriate.
The now recommended Xpert MTB/ RIF-test may be quite useful for rapid detection of TB in lymph node aspirates..
However,it cannot replace the need for TB culture to detect MDR- and XDR-TB, as it can only detect Rifampicin- resistance, which alone is not sufficient to qualify for MDR-TB, and the test contributes nothing for the detection of XDR-TB.
Moreover, this test gives a false negative result, if resistance is present not aginst Rifampicin, but instead against two of the other drugs in use for first line TB-treatment (see Lancet 2011 Vol 377, 1467) .
Conclusions
This method of fine needle lymph node aspiration shows, that even without culture medium in place, the yield is impressive, and, in combination with cytology, excellent results can be expected.
Moreover a sensitivity testing can be carried out, thus enabling the detection of MDR- and XDR - TB
Further improvement may be possible by doing two aspirates, to increase the amount of specimen for the culture.
This technique of aspirates - at least from peripheral lymph nodes - is simple and can even be performed by trained nurses in small hospitals and clinics.
See the 2nd study of 545 patients
 Lymph node aspirates in Tuberculosis-Diagnosis: New challenges, new solutions – a second study of 545 patients
Lymph node aspirates in Tuberculosis-Diagnosis: New challenges, new solutions – a second study of 545 patients
 Lymph node aspirates in Tuberculosis-Diagnosis - A third study of 549 patients
Lymph node aspirates in Tuberculosis-Diagnosis - A third study of 549 patients
 Diagnosis of disseminated Tuberculosis in bone marrow aspirates
Diagnosis of disseminated Tuberculosis in bone marrow aspirates
.
avonpaleske@yahoo.de
1) Pithie AD, Chicksen B.
Fine-needle extrathoracic lymph-node aspiration in HIV-associated sputum-negative tuberculosis, Lancet. 1992 Dec 19-26;340(8834-8835):1504-5
2) Dandapat, M.C. B. M. Mishra, S. P. Dash, P. K. Kar
Peripheral lymph node tuberculosis: A review of 80 cases British Journal of Surgery
Vol. 77, pp. 911–912, 1990
3)Scott K. Heysell, Anthony P. Moll, Neel R. Gandhi, François J. Eksteen, Palav Babaria, Yacoob Coovadia, Lynn Roux, Umesh Lalloo, Gerald Friedland, and N. Sarita Shah
-Extensively Drug-Resistant Mycobacterium tuberculosis from Aspirates, Rural South Africa--- CDC-EID Vol. 16 No 3, March 2010
Mpilo-Hospital
Teaching Hospital of the University of Zimbabwe
Bulawayo/Zimbabwe
Africa
Introduction
Lymph node tuberculosis is not infrequent in Sub-Saharan Africa. Even though precise figures do not exist, the incidence can be estimated to be between 10 and 25% of all TB cases..
A few studies have been published which show the value of fine needle aspiration for the diagnosis of lymph node TB, albeit with small numbers. The results were, apart from a few exceptions based on microscopy only.
In the meantime new challenges have arisen:
1. 3% of all Tuberculosis cases worldwide are multidrug resistant (MDR-TB), in certain affected areas the percentage is, however, much higher. Thus the diagnosis for MDR-TB in lymph node TB becomes extremely important. The extensive drug resistant TB (XDR-TB) is on the rise as well..
2. The HIV epidemic has brought more challenges for the diagnosis of lymph node TB
- Many patients present with enlarged lymph nodes of which it is unclear, whether this is TB, or persistent generalized HIV-related lymph node enlargement
- Other infectious diseases like Histoplasmosis and Cryptococcal infections, or simple bacterial lymphadenitis can present with lymph node enlargement as well
- The same applies to HIV-related cancers presenting with lymph node enlargement (Kaposi-Sarcoma, high grade Non Hodgkin lymphoma, Hodgkin´s disease, Castleman's disease).
- HIV-positive patients, who are on anti-TB-treatment (ATT) for lymph node TB, and who have been started concurrently or shortly before on treatment with antiretroviral drugs, can show increasing, or at least persistent lymph node enlargement, which may be in fact not drug resistant TB, but part of an Immune-Reconstitution Syndrome (IRS) or newly developed high grade lymphoma.
- The new WHO recommendations for TB-prophylaxis in HIV-positive patients - INH for a period of at least 6 months - require the exclusion of active TB, which is clinically often not possible in view of the frequently enlarged lymph nodes in HIV-positive patients.
The gold standard for a definitive diagnosis is certainly a lymph node biopsy. However this is in most of Sub-Saharan Africa, due to lack of facilities and manpower, at present only feasible for a very small number of patients.
Lymph node aspirates on the other hand are simple to perform, the specimen obtained can easily be spread on slides and then assessed by a laboratory technologist .
However, the microscopy result is often negative for TB-bacilli (AAFBs, Alcohol and Acid fast Bacilli), especially in fairly immune-competent patients, unlike with sputum in cases of TB lung,.
Helpful in the diagnosis of lymph node TB, despite the absence of microscopically detectable TB-Bacilli, is the detection of caseous material and / or the presence of Langhans giant cells.
,
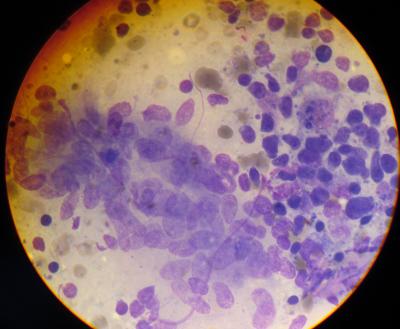
Langhans Giant cell in a lymph node aspirate - Photo: Dr. v. Paleske
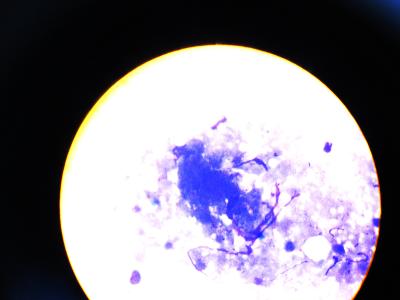
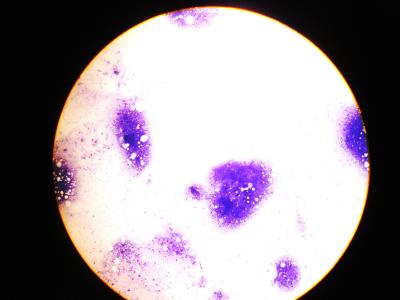
Caseous material in lymph node aspirate - Photos: Dr. v. Paleske
In our setting 25% of all lymph node aspirate specimens were falling into this category (unpublished data.). Culture of these aspirates would help further in the diagnosis of TB
In contrast: the lymph node aspirates of severely immune-compromised patients are often pus-like, packed with AAFBs and can thus fairly easily be diagnosed under the microscope.
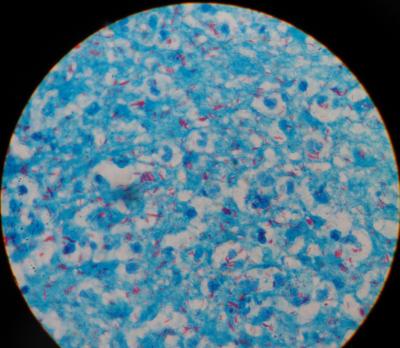
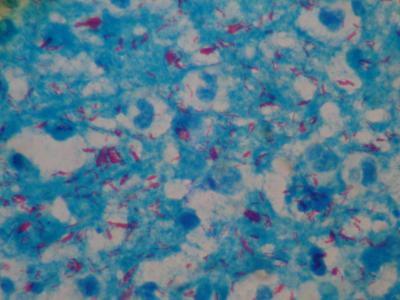
Lymph node TB, plentiful AAFBs, full blown AIDS - Photo: Dr. v. Paleske
Moreover, In view of the increasing numbers of MDR-TB and XDR-TB, culture and sensitivity testing should be done, whenever possible.
The problems: amount of specimen and mode of transport / culture medium.
For lymph node aspirates this poses a challenge, as the amount of specimen obtained with a fine needle aspirate is often little. Moreover TB-culture-medium is not available in district hospitals and clinics.
We have investigated a way to solve this problem, which allows the aspirate firstly to be spread on a slide for microscopy diagnosis and also sent off for TB culture as well.
Patients and methods
129 patients age 15 – 85 years and 27 pat. age 2 months to 14 years were referred to Mpilo-Hospital Bulawayo / Zimbabwe for fine needle aspirate of enlarged peripheral or paraarotic/parailiacal/abdominal lymph nodes during the period from 1st May 2010 to 30th April 2011.
None of the patients had a formal lymph node biopsy before.
Aspirates were performed with a 5ml or 10 ml syringe. For peripheral lymph nodes size 18 or 19 G needles were used, however for abdominal or paraaortal /parailiacal lymph node aspirates the smaller size 21 G needles.
The specimens were spread on a glass slide and a quash smear with another glass slide facilitated. This technique is better in preserving fragments and thus allows better the recognition of caseous material.
Thereafter a blood sample was taken from the patient and 1 - 1,5ml blood filled in an EDTA-Tube (Full blood count tube).
The aspirate syringe with the aspirate needle on top was flushed several times with the blood in the EDTA-tube by sucking the blood into the aspirate syringe an pressing it back into the EDTA tube, thus delivering the rest of the specimen into the EDTA-tube.
The EDTA tube was then sent to the TB-Lab for TB-culture.
May- Gruenwald Giemsa staining was being done on one glass slide, Ziehl-Neelsen for detection of AAFBs on the other.
Results
Altogether the diagnosis TB was made in 79 of the 156 specimens (50.6%)
1. Microscopically positive for TB (Langhans Giant Cells and / or caseation and / or AAFBs detected) were 62 / 79 (78,4%), of which 36 / 79 (45%) were microscopically AAFBs-positive
2. TB-Culture positive were 52/79 (65,8% of all TB diagnoses) all m. tuberculosis.
In Detail:
-- Culture positive, plus microscopically positive including AAFBs detected were 27 / 79 (34,1%)
- Culture positive plus microscopically caseation and / or Langhans giant cells but no AAFBs microscopically detected were 12 / 79 (15,1%)
- Culture positive “only” , microscopically no evidence of TB (neither AAFB's detected, nor caseation, nor Langhans giant cells were found, instead a reactive pattern) was seen in 13 / 79 specimens (16,4%)
- Culture negative but microscopically positive plus AAFBs detected were 9 /79 (11,3%)
- Culture negative, but microscopically positive however no AAFBs detected were 18 / 79 (22,7%)
Discussion
The aspirate-specimens from lymph nodes mixed with 1-1,5 ml of EDTA-Blood from the patient, had an acceptable yield.
We, however, did not separate the patients, who are on Anti TB drugs, and for how long, or not at all.
Patients, whose aspirates are microscopically AAFB´s negative, culture negative but were diagnosed on the basis of caseation, or pus, or Langhans giant cells, without the presence of Non-TB bacilli, and without a significant amount of granulocytes or macrophages, who are either for weeks on anti-TB-drugs or have recently completed their TB treatment cannot outright be regarded as therapeutic failures.
Therefore a change of treatment (switch to 2nd line TB treatment) seems not justified, rather a “wait and see policy” should be pursued with a second aspirate in due course.
.
Those however, whose aspirates are microscopically AAFBs positive, not on ATT and culture negative are definitely culture falsely negative and need treatment. A repeat aspirate solely for culture may be appropriate.
The now recommended Xpert MTB/ RIF-test may be quite useful for rapid detection of TB in lymph node aspirates..
However,it cannot replace the need for TB culture to detect MDR- and XDR-TB, as it can only detect Rifampicin- resistance, which alone is not sufficient to qualify for MDR-TB, and the test contributes nothing for the detection of XDR-TB.
Moreover, this test gives a false negative result, if resistance is present not aginst Rifampicin, but instead against two of the other drugs in use for first line TB-treatment (see Lancet 2011 Vol 377, 1467) .
Conclusions
This method of fine needle lymph node aspiration shows, that even without culture medium in place, the yield is impressive, and, in combination with cytology, excellent results can be expected.
Moreover a sensitivity testing can be carried out, thus enabling the detection of MDR- and XDR - TB
Further improvement may be possible by doing two aspirates, to increase the amount of specimen for the culture.
This technique of aspirates - at least from peripheral lymph nodes - is simple and can even be performed by trained nurses in small hospitals and clinics.
See the 2nd study of 545 patients
.
avonpaleske@yahoo.de
1) Pithie AD, Chicksen B.
Fine-needle extrathoracic lymph-node aspiration in HIV-associated sputum-negative tuberculosis, Lancet. 1992 Dec 19-26;340(8834-8835):1504-5
2) Dandapat, M.C. B. M. Mishra, S. P. Dash, P. K. Kar
Peripheral lymph node tuberculosis: A review of 80 cases British Journal of Surgery
Vol. 77, pp. 911–912, 1990
3)Scott K. Heysell, Anthony P. Moll, Neel R. Gandhi, François J. Eksteen, Palav Babaria, Yacoob Coovadia, Lynn Roux, Umesh Lalloo, Gerald Friedland, and N. Sarita Shah
-Extensively Drug-Resistant Mycobacterium tuberculosis from Aspirates, Rural South Africa--- CDC-EID Vol. 16 No 3, March 2010
onlinedienst - 30. Aug, 14:35 Article 24362x read